Aims: The aim of the study was to describe a cohort of patients reoperated on for persistent primary macular hole, and to evaluate the anatomical and functional results of the reoperated patients.
Material and Methods: 459 eyes of 390 patients were operated on for primary macular hole at Department of Ophthalmology, 3rd Faculty of Medicine, Charles University, Kralovske Vinohrady University Hospital between January 1, 2013, and December 31, 2023. We included 33 eyes of 33 patients in our retrospective case series, in which macular hole persisted after the primary surgery. Preoperative, perioperative and postoperative data of these patients were recorded, as well as initial and resulting best corrected visual acuity (BCVA), surgical technique, whether the first or second reoperation was successful. The minimum follow-up time was 90 days after the revision surgery. The statistical analysis included descriptive statistics to characterize the demographic and clinical parameters. Qualitative and quantitative variables were analyzed using means, medians and standard deviations.
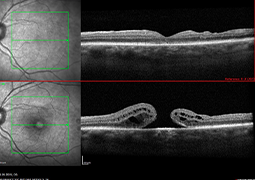
Results: Primary surgery for macular holes was successful in 426 eyes of 357 patients (92.8%). The surgery was unsuccessful in the remaining 33 eyes of 33 patients (7.2%), with persistent macular hole. These patients underwent reoperation, which led to closure of the hole in 27 of 33 eyes (reoperation success rate 81.8% and total success rate of primary surgery and reoperation altogether 98.7%). Reoperation was unsuccessful in 6 eyes (18.2% of reoperated eyes and 1.3% of all operated macular holes). In 4 eyes a second reoperation was performed; in 3 eyes the reoperation was successful and led to an improvement of BCVA. The average BCVA of the successfully reoperated eyes was 65.2 ± 11.9 letters (ETDRS ±SD). In the eyes of patients after a successful second reoperation, BCVA was 56.7 ±8.4 letters, while in the eyes of patients who did not undergo further surgery (n = 3), average BCVA was only 39.0 ±11.0 letters.
Conclusion: Reoperation of macular holes has a very good success rate and usually leads to an improvement of visual acuity. Improvement of visual acuity can also be achieved in patients who only achieved success after a second reoperation.